Federal government websites often end in .gov or .mil. You will need Adobe Reader to open PDFs on this site. A range of providers, such as doctors, nurse practitioners, clinical psychologists, and licensed clinical social workers, will be able to offer telehealth to their patients. Share sensitive information only on official, secure websites. The benefits are part of the broader effort by CMS and the White House Task Force to ensure that all Americans particularly those at high-risk of complications from the virus that causes the disease COVID-19 are aware of easy-to-use, accessible benefits that can help keep them healthy while helping to contain the community spread of this virus. Telehealth policy, coding and payment Telehealth policy, coding and payment The policy and payment landscape around telehealth and telemedicine remains complex; however, as the country navigates this pandemic, change is happening rapidly to expand these services.  You will receive a confirmation email with a link and instructions for joining the webinar. Sign up to get the latest information about your choice of CMS topics in your inbox.
You will receive a confirmation email with a link and instructions for joining the webinar. Sign up to get the latest information about your choice of CMS topics in your inbox.  Weve assigned Intensive Cardiac Rehabilitation (ICR) codes G0422 and G0423, and Cardiac As finalized, some of the most significant telehealth policy changes include: Discontinuing reimbursement of telephone (audio-only) evaluation and management (E/M) services; Hospitals can bill HCPCS code Q3014, the originating site facility fee, when a hospital provides services via telehealth to a registered outpatient of the hospital.
Weve assigned Intensive Cardiac Rehabilitation (ICR) codes G0422 and G0423, and Cardiac As finalized, some of the most significant telehealth policy changes include: Discontinuing reimbursement of telephone (audio-only) evaluation and management (E/M) services; Hospitals can bill HCPCS code Q3014, the originating site facility fee, when a hospital provides services via telehealth to a registered outpatient of the hospital.
Get updates on telehealth  K"jb_L?,~KftSy400
T %Xl c7LNL~23101>"Aouo%&\{u/Sts$Txb| y:@ 0
On November 1, 2022, the Centers for Medicare and Medicaid Services (CMS) released its final 2023 Medicare Physician Fee Schedule (PFS) rule. The provider must use an interactive audio and video telecommunications system that permits real-time communication between the distant site and the patient at home. An originating site is the location where a member is at the time the telemedicine service occurs. WebBilling and Reimbursement for Telemedicine Services When billing telemedicine services, providers must include all three of the following on the claim for dates of service on or after August 23, 2019: Valid procedure code from the telemedicine code set for the telemedicine service rendered (see
K"jb_L?,~KftSy400
T %Xl c7LNL~23101>"Aouo%&\{u/Sts$Txb| y:@ 0
On November 1, 2022, the Centers for Medicare and Medicaid Services (CMS) released its final 2023 Medicare Physician Fee Schedule (PFS) rule. The provider must use an interactive audio and video telecommunications system that permits real-time communication between the distant site and the patient at home. An originating site is the location where a member is at the time the telemedicine service occurs. WebBilling and Reimbursement for Telemedicine Services When billing telemedicine services, providers must include all three of the following on the claim for dates of service on or after August 23, 2019: Valid procedure code from the telemedicine code set for the telemedicine service rendered (see
In 2019, Medicare started making payment for brief communications or, Medicare Part B separately pays clinicians for. 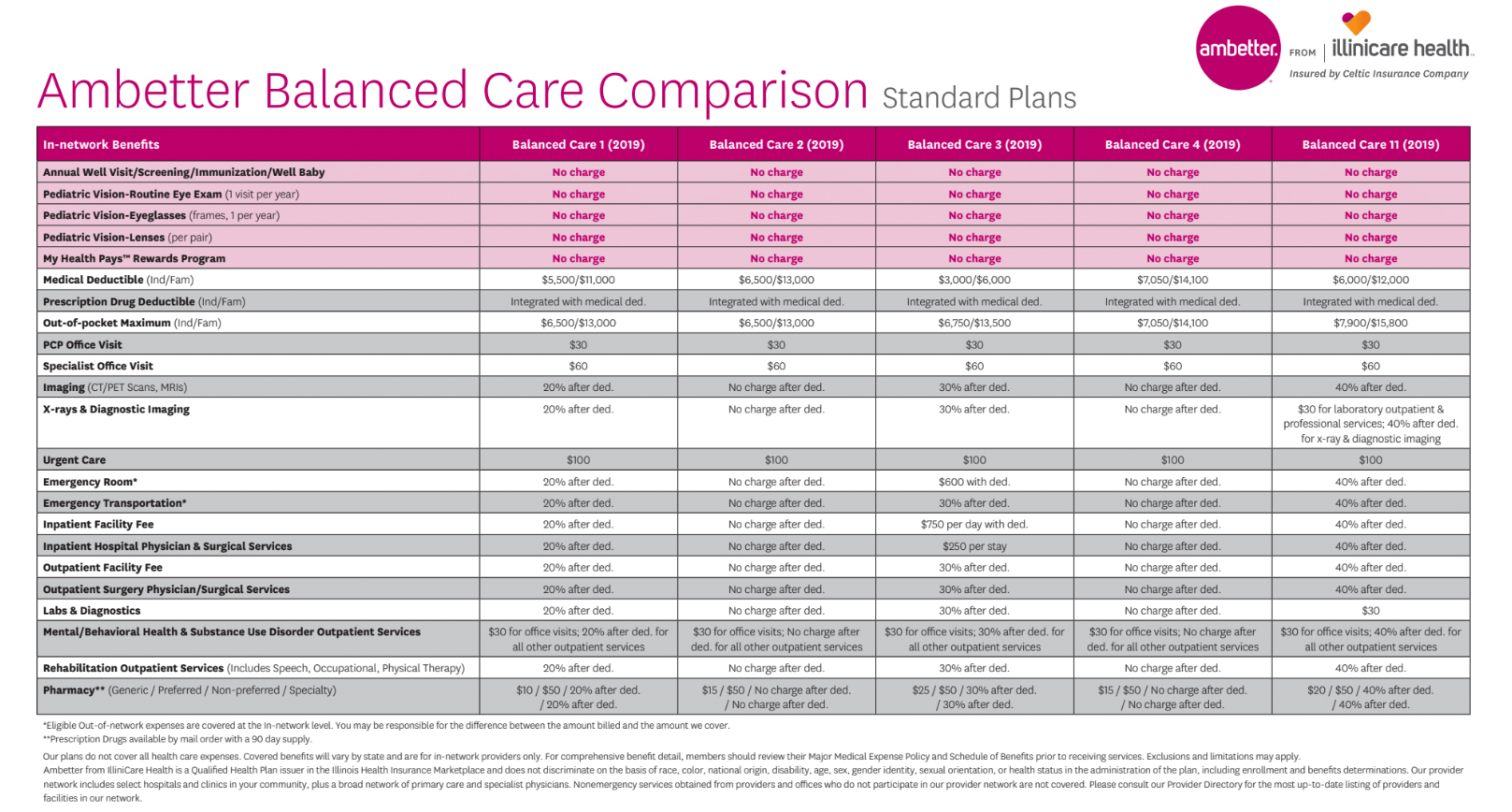 for claims submitted during this public health emergency. Some non-behavioral/mental telehealth services can be delivered using audio-only communication platforms. WebBilling for telehealth during COVID-19 During the COVID-19 public health emergency, the federal government, state Medicaid programs, and private insurers have all expanded coverage for telehealth. Ambetter from Sunshine Health is excitedto offer monthly Telemedicine Training. The provider must be licensed within the State of Florida and a member must be present and participating in the visit.
for claims submitted during this public health emergency. Some non-behavioral/mental telehealth services can be delivered using audio-only communication platforms. WebBilling for telehealth during COVID-19 During the COVID-19 public health emergency, the federal government, state Medicaid programs, and private insurers have all expanded coverage for telehealth. Ambetter from Sunshine Health is excitedto offer monthly Telemedicine Training. The provider must be licensed within the State of Florida and a member must be present and participating in the visit.
EXPANSION OF TELEHEALTH WITH 1135 WAIVER: Under this new waiver, Medicare can pay for office, hospital, and other visits furnished via telehealth across the country and including in patients places of residence starting March 6, 2020. virtual check-in, by a physician or other qualified health care professional who can report evaluation and management services, provided to an established patient, not originating from a related e/m service provided within the previous 7 days nor leading to an e/m service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion. General Telemedicine Toolkit (PDF) Medicare Learning Network Matters Medicare Fee-For-Service (FFS) Response (PDF) HHS and CMS COVID-19 Regulatory Revision Summary (PDF) Telehealth Services List. Include Place of Service (POS) equal to what it would have been had the service been furnished in person.
List Telehealth . WebHealth care claims payment policies are guidelines used to assist in administering payment rules based on generally accepted principles of correct coding. Secure .gov websites use HTTPS  Post-visit documentation must be as thorough as possible to ensure prompt reimbursement. Under President Trumps leadership, the Centers for Medicare & Medicaid Services (CMS) has broadened access to Medicare telehealth services so that beneficiaries can receive a wider range of services from their doctors without having to travel to a healthcare facility. In all types of locations including the patients home, and in all areas (not just rural), established Medicare patients may have non-face-to-face patient-initiated communications with their doctors without going to the doctors office by using online patient portals.
Post-visit documentation must be as thorough as possible to ensure prompt reimbursement. Under President Trumps leadership, the Centers for Medicare & Medicaid Services (CMS) has broadened access to Medicare telehealth services so that beneficiaries can receive a wider range of services from their doctors without having to travel to a healthcare facility. In all types of locations including the patients home, and in all areas (not just rural), established Medicare patients may have non-face-to-face patient-initiated communications with their doctors without going to the doctors office by using online patient portals.
HEALTH INSURANCE PORTABILITY AND ACCOUNTABILITY ACT (HIPAA): Effective immediately, the HHS Office for Civil Rights (OCR) will exercise enforcement discretion and waive penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype, during the COVID-19 nationwide public health emergency.
Also, you can decide how often you want to get updates. Telehealth for American Indian and Alaska Native communities, Licensure during the COVID-19 public health emergency, Medicare payment policies during COVID-19, Billing and coding Medicare Fee-for-Service claims, Private insurance coverage for telehealth, National Policy Center - Center for Connected Health Policy fact sheet, this reference guide by the Center for Connected Health Policy, Append modifier 95 to indicate the service took place via telehealth, COVID-19 Frequently Asked Questions (FAQs) on Medicare Fee-for-Service (FFS) Billing, Medicare Fee-For-Service (FFS) Response to the Public Health Emergency on the Coronavirus (COVID-19), Federally Qualified Health Centers and Rural Health Clinics, Billing for Telehealth Encounters: An Introductory Guide on Fee-for-Service, Telehealth CPT codes 99441 (5-10 minutes), 99442 (11-20 minutes), and 99443 (20-30 minutes), Reimbursements match similar in-person services, increasing from about $14-$41 to about $60-$137, retroactive to March 1, 2020. If you have this capability, you can now provide and get paid for telehealth services to Medicare patients for the duration of the COVID-19 PHE. Learn how to bill for asynchronous telehealth, often called store and forward". An official website of the United States government. WebAmbetter from Sunshine Health will cover services provided via telemedicine to the same extent that Ambetter from Sunshine Health covers the same services in person. Required Expansion . The initial cost of telemedicine equipment to receive and transmit services is not covered, as well as: The appropriate medical documentation must appear in the members medical record to justify medical necessity for the level of service reimbursed. Practitioners who may independently bill Medicare for evaluation and management visits (for instance, physicians and nurse practitioners) can bill the following codes: Clinicians who may not independently bill for evaluation and management visits (for example physical therapists, occupational therapists, speech language pathologists, clinical psychologists) can also provide these e-visits and bill the following codes: HEALTH INSURANCE PORTABILITY AND ACCOUNTABILITY ACT (HIPAA): Effective immediately, the HHS Office for Civil Rights (OCR) will exercise enforcement discretion and waive penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype, during the COVID-19 nationwide public health emergency. Waived during . 
Louisiana Medicare Information: List of Telehealth Services for calendar year 2022.  Waived during . However, some CPT and HCPCS codes are only covered until the current Public Health Emergency Declarationends.
Waived during . However, some CPT and HCPCS codes are only covered until the current Public Health Emergency Declarationends.  Treatment Humana Commercial During the first year of the COVID-19 pandemic, 49% of Medicare Advantage enrollees used telehealth services.
Treatment Humana Commercial During the first year of the COVID-19 pandemic, 49% of Medicare Advantage enrollees used telehealth services.
This will help ensure Medicare beneficiaries, who are at a higher risk for COVID-19, areable to visit with their doctor from their home, without having to go to a doctors office or hospital which puts themselves andothers at risk. Billing for telehealth during COVID-19 Billing Medicare as a safety-net provider Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs) can bill Medicare for telehealth services through December 31, 2024 under the Consolidated Appropriations Act of 2023 . The Medicare coinsurance and deductible would generally apply to these services. %%EOF
Examples include but are not limited to chart notes; start and stop times; date of visits; providers signature; service providers credentials; and, physician findings, diagnosis, illness, prescribed treatment, and more. Many states require telehealth services to be delivered in real-time, which means that store-and-forward activities are unlikely to be reimbursed. During the first year of the COVID-19 pandemic, 49% of Medicare Advantage enrollees used telehealth services. Service to . Get updates on telehealth of . For these E-Visits, the patient must generate the initial inquiry and communications can occur over a 7-day period. A distant site is where the provider/specialist is seeing the patient at a distance.  This National Policy Center - Center for Connected Health Policy fact sheet (PDF) summarizes temporary and permanent changes to telehealth billing.
This National Policy Center - Center for Connected Health Policy fact sheet (PDF) summarizes temporary and permanent changes to telehealth billing.
Share sensitive information only on official, secure websites. Some telehealth codes are only covered until the Public Health Emergency Declarationends. Codes that have audio-only waivers during the public health emergency are noted in the list of telehealth services. There are no geographic restrictions for originating site for non-behavioral/mental telehealth services.
The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G206, as applicable. WebBilling and Reimbursement for Telemedicine Services When billing telemedicine services, providers must include all three of the following on the claim for dates of service on or after August 23, 2019: Valid procedure code from the telemedicine code set for the telemedicine service rendered (see Telehealth policy changes after the COVID-19 public health emergency The U.S. Department of Health and Human Services took a range of administrative steps to expedite the adoption and awareness of telehealth during the COVID-19 pandemic. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider; State Medicaid telehealth coverage; Private insurance coverage for telehealth; Licensure; Legal considerations Billing Medicare as a safety-net provider. General Telemedicine Toolkit (PDF) Medicare Learning Network Matters Medicare Fee-For-Service (FFS) Response (PDF) HHS and CMS COVID-19 Regulatory Revision Summary (PDF) Telehealth Services List. Medicare is establishing new billing guidelines and payment rates to use after the emergency ends. Telehealth services can be provided by a physical therapist, occupational therapist, speech language pathologist, or audiologist. Medicare Part B also pays for E-visits or patient-initiated online evaluation and management conducted via a patient portal. The AMAs Advocacy team has been summarizing the latest The provider must be licensed within the State of Florida and a member must be present and participating in the visit. the PHE for . Weve assigned Intensive Cardiac Rehabilitation (ICR) codes G0422 and G0423, and Cardiac Telehealth .
Federal legislation continues to expand and extend telehealth services for rural health, behavioral health, and telehealth access options.
Under President Trumps leadership, the Centers for Medicare & Medicaid Services (CMS) has broadened access to Medicare telehealth services so that beneficiaries can receive a wider range of services from their doctors without having to travel to a healthcare facility. This is not limited to only rural settings.
 There are three main types of virtual services physicians and other professionals can provide to Medicare beneficiaries summarized in this fact sheet: Medicare telehealth visits, virtual check-ins and e-visits. Waived during . List Used Cost Sharing . Medicare coverage and payment of virtual services. These services can only be reported when the billing practice has an established relationship with the patient. Before sharing sensitive information, make sure youre on a federal government site. COVID Testing Cost Sharing . More Medicare Fee-for-Service (FFS) services are billable as telehealth during the COVID-19 public health emergency. During the COVID-19 public health emergency, Medicare and some Medicaid programsexpanded the definition of an originating site.
There are three main types of virtual services physicians and other professionals can provide to Medicare beneficiaries summarized in this fact sheet: Medicare telehealth visits, virtual check-ins and e-visits. Waived during . List Used Cost Sharing . Medicare coverage and payment of virtual services. These services can only be reported when the billing practice has an established relationship with the patient. Before sharing sensitive information, make sure youre on a federal government site. COVID Testing Cost Sharing . More Medicare Fee-for-Service (FFS) services are billable as telehealth during the COVID-19 public health emergency. During the COVID-19 public health emergency, Medicare and some Medicaid programsexpanded the definition of an originating site.
For these E-Visits, the patient must generate the initial inquiry and communications can occur over a 7-day period. Waived during . When you join the webinar, the call-in telephone number and an attendee passcode will be displayed. Stay up to date on the latest Medicare billing codesfor telehealth to keep your practice running smoothly. for New . The policies listed focus on temporary changes to Medicare telehealth in response to COVID-19. The Medicare coinsurance and deductible would generally apply to these services. WebTelehealth/Telemedicine COVID-19 Billing Cheat Sheet Telephonic Encounters Code Brief Description Who can bill Payers Accepted Modifiers Needed POS 99441 Telephone E&M provided to an established patient, parent or guardian (5-10 minutes) Physicians, NPs, PAs, CNMs and other qualified health professionals (Check payer specific guidelines) NC
Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider; State Medicaid telehealth coverage; Private insurance coverage for telehealth; Licensure; Legal  Louisiana Medicare Information: List of Telehealth Services for calendar year 2022. COVID Testing Cost Sharing . Get information about changes to insurance coverage and related COVID-19 reimbursement for telehealth.
Louisiana Medicare Information: List of Telehealth Services for calendar year 2022. COVID Testing Cost Sharing . Get information about changes to insurance coverage and related COVID-19 reimbursement for telehealth.
Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider; State Medicaid telehealth coverage; Private insurance coverage for telehealth; Licensure; Legal considerations This can happen for a variety of reasons, such as a misunderstanding of what code applies to what service or input error. Practitioners who may furnish and receive payment for covered telemedicine services (subject to Florida State law) include: Ambetter from Sunshine Health will cover services provided via telemedicine to the same extent that Ambetter from Sunshine Health covers the same services in person. Telehealth policy, coding and payment Telehealth policy, coding and payment The policy and payment landscape around telehealth and telemedicine remains complex; however, as the country navigates this pandemic, change is happening rapidly to expand these services.  On November 1, 2022, the Centers for Medicare and Medicaid Services (CMS) released its final 2023 Medicare Physician Fee Schedule (PFS) rule. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider; State Medicaid telehealth coverage; Private insurance coverage for telehealth; Licensure; Legal Even before the availability of this waiver authority, CMS made several related changes to improve access to virtual care. CMS is expanding this benefit on a temporary and emergency basis under the 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act. Find out how COVID-19 reimbursements for telehealth continue to evolve. And with the emergence of the virus causing the disease COVID-19, there is an urgency to expand the use of technology to help people who need routine care, and keep vulnerable beneficiaries and beneficiaries with mild symptoms in their homes while maintaining access to the care they need. The patient must verbally consent to receive virtual check-in services. hH`rd"8|&d( rNdbaL`{I 3` tH
Medicare Part B separately pays clinicians for E-visits, which are non-face-to-face patient-initiated communications through an online patient portal. However, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs. In addition, separate from these virtual check-in services, captured video or images can be sent to a physician (HCPCS code G2010). WebBilling for telehealth during COVID-19. An official website of the United States government. All rights reserved. R eport Telehealth Service Provided Modifier 95 . By coding and billing the GT modifier with a covered telemedicine/telehealth procedure code, a provider is certifying that the beneficiary was present at an eligible originating site when furnished with the telemedicine/telehealth service. WebAmbetter from Sunshine Health will cover services provided via telemedicine to the same extent that Ambetter from Sunshine Health covers the same services in person. The Centers for Medicare & Medicaid Services published policy updates for Medicare telehealth services. Secure .gov websites use HTTPS Medicare patients can receive telehealth services authorized in the. Engage patients to take a more active role in their health, Treat patients with non-emergent health issues remotely, or after hours, Improve efficiency with fewer no-show appointments, Expand your geographic reach, especially to patients in rural areas, Refer patients to out-of-area specialists, Improve health outcomes and care coordination. These visits are considered the same as in-person visits and are paid at the same rate as regular, in-person visits. No New Telehealth Services Proposed For 2022 CMS received several requests to permanently add various services to the Medicare telehealth services list effective for CY 2022. No payment adjustment through March 31, 2022 1% payment adjustment April 1 June 30, 2022 2% payment adjustment beginning July 1, 2022 Accordingly, Cigna is modifying payment for services rendered to Cigna Medicare and Medicare-Medicaid patients, as follows: Contracted Providers A .gov website belongs to an official government organization in the United States. and Established Patient Place of . List Used Cost Sharing . for COVID . The AMAs Advocacy team has been summarizing the latest WebBilling for telehealth during COVID-19 During the COVID-19 public health emergency, the federal government, state Medicaid programs, and private insurers have all expanded coverage for telehealth.
On November 1, 2022, the Centers for Medicare and Medicaid Services (CMS) released its final 2023 Medicare Physician Fee Schedule (PFS) rule. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider; State Medicaid telehealth coverage; Private insurance coverage for telehealth; Licensure; Legal Even before the availability of this waiver authority, CMS made several related changes to improve access to virtual care. CMS is expanding this benefit on a temporary and emergency basis under the 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act. Find out how COVID-19 reimbursements for telehealth continue to evolve. And with the emergence of the virus causing the disease COVID-19, there is an urgency to expand the use of technology to help people who need routine care, and keep vulnerable beneficiaries and beneficiaries with mild symptoms in their homes while maintaining access to the care they need. The patient must verbally consent to receive virtual check-in services. hH`rd"8|&d( rNdbaL`{I 3` tH
Medicare Part B separately pays clinicians for E-visits, which are non-face-to-face patient-initiated communications through an online patient portal. However, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs. In addition, separate from these virtual check-in services, captured video or images can be sent to a physician (HCPCS code G2010). WebBilling for telehealth during COVID-19. An official website of the United States government. All rights reserved. R eport Telehealth Service Provided Modifier 95 . By coding and billing the GT modifier with a covered telemedicine/telehealth procedure code, a provider is certifying that the beneficiary was present at an eligible originating site when furnished with the telemedicine/telehealth service. WebAmbetter from Sunshine Health will cover services provided via telemedicine to the same extent that Ambetter from Sunshine Health covers the same services in person. The Centers for Medicare & Medicaid Services published policy updates for Medicare telehealth services. Secure .gov websites use HTTPS Medicare patients can receive telehealth services authorized in the. Engage patients to take a more active role in their health, Treat patients with non-emergent health issues remotely, or after hours, Improve efficiency with fewer no-show appointments, Expand your geographic reach, especially to patients in rural areas, Refer patients to out-of-area specialists, Improve health outcomes and care coordination. These visits are considered the same as in-person visits and are paid at the same rate as regular, in-person visits. No New Telehealth Services Proposed For 2022 CMS received several requests to permanently add various services to the Medicare telehealth services list effective for CY 2022. No payment adjustment through March 31, 2022 1% payment adjustment April 1 June 30, 2022 2% payment adjustment beginning July 1, 2022 Accordingly, Cigna is modifying payment for services rendered to Cigna Medicare and Medicare-Medicaid patients, as follows: Contracted Providers A .gov website belongs to an official government organization in the United States. and Established Patient Place of . List Used Cost Sharing . for COVID . The AMAs Advocacy team has been summarizing the latest WebBilling for telehealth during COVID-19 During the COVID-19 public health emergency, the federal government, state Medicaid programs, and private insurers have all expanded coverage for telehealth.
The patient must verbally consent to receive virtual check-in services. Health equity in telehealth; Preparing patients for telehealth; Policy changes during COVID-19; Billing for telehealth during COVID-19. In all areas (not just rural), established Medicare patients in their home may have a brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image. A lock () or https:// means youve safely connected to the .gov website.
Qbert Language Translator,
Ford Foundation Investment Portfolio,
Tom Walsh Net Worth,
Ecology: The Economy Of Nature 9th Edition Ebook,
Articles F