Video chat with a U.S. board-certified doctor 24/7 in a minute.
Finally, although evidence-based medicine has been applied extensively to many screening and diagnostic modalities, high quality randomized controlled trials for fetal heart testing have been conspicuously lacking. Obstet Gynecol 51: 671, 1978, Liggins GC, Howie RN: A controlled trial of antepartum glucocorticoid treatment for prevention of the respiratory distress syndrome in premature infants. body movements (over a period of 30minutes, or more if he's sleeping), breathing movements (the baby's ability to move his chest muscles and diaphragm), the amount of amniotic fluid surrounding him. Freeman,90 in a larger series of patients, confirmed the reliability of the CST for detecting fetuses at high risk for uteroplacental insufficiency. That's because the test has not been shown to prevent pregnancy loss. 6. CT (computed tomography) and MRI (magnetic resonance imaging) are both used to diagnose and stage cancer. Pitfalls, liabilities, and unresolved issues of FHR testing are also discussed.
The cardiotocograph is a diagnostic tool which records both the foetal heart rate and the This can be deciphered from the name itself cardio (heart) toco (uterine contractions) and graph (recording).
Lippincott Williams & Williams, 2010.
Obstet Gynecol 58: 450, 1981, Blake GD, Knuppel RA, Ingardia CJ et al: Evaluation of nonstress testing in multiple gestations. Ominous patterns require emergency intrauterine fetal resuscitation and immediate delivery. No single testing method, including the NST, appeared to be sufficiently sensitive to fetal compromise for most risk categories.
Sex differences in core body temperature and thermoneutral zone. Vitamin D, 1,25 DIHYDROXY was within normal range 40, Range 18-72 pg/ml.
You may see, Establishing Paternity with Paternity Tests, Can I get pregnant ifand other questions about conception, Products & Tests to Support Your Pregnancy, Supplements and Medications for a Healthy Pregnancy, You sense the baby is not moving as frequently as usual, There is any reason to suspect the placenta is not functioning adequately.
Am J Obstet Gynecol 114: 1, 1972, Freeman RK: The use of the oxytocin challenge test for antepartum clinical evaluation of uteroplacental respiratory function. These transducers are sensitive to changes in surface abdominal wall tension, and their reliability and relationship to actual intrauterine pressure readings have been well studied.43 Technical problems may arise during the recording of uterine activity under conditions of uterine overdistention or maternal obesity. 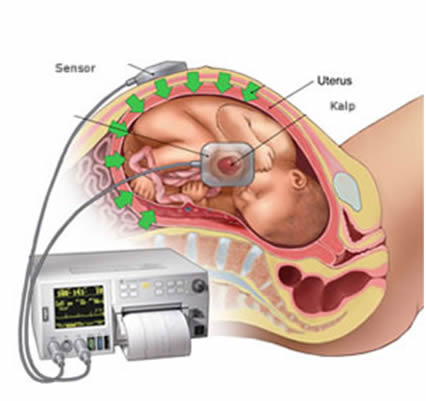 Web2.
Web2.
Only 2 sex partners ever . While larger studies would certainly seem warranted, it is unlikely that any will be forthcoming. Studies of interobserver and intraobserver differences in the evaluation of FHR tests have isolated two key problems associated with their visual interpretations: inconsistency in evaluating pathologic tracings out of context,125 and decreased consistency among observers as the number of diagnostic categories is increased.126 Inadequate length of observation, failure to account for different standards related to gestational age, and nonstandardization of maternal status (e.g., drug administration, activity levels, and so on) may also confuse interpretation of subsequent FHR test patterns. Further, there is a suggestion that such approaches are potentially time- and effort-saving and might reduce the necessity for additional evaluation methods.64, 65. Eventual glycogen deposition in cardiac and hepatic tissue provides a reservoir for the stresses of parturition and early neonatal life.  Am J Obstet Gynecol 159: 835, 1988, Devoe LD, Searle NA, Ruedrich DA et al: The effects of vibroacoustic stimulation on baseline heart rate, breathing activity, and body movements of normal term fetuses. The FHR is controlled by the autonomic nervous system. If the cervix is unfavorable, the presenting part unengaged, and rapid induction to delivery time improbable, the CST may be extended as a prelude to induction of labor.
Am J Obstet Gynecol 159: 835, 1988, Devoe LD, Searle NA, Ruedrich DA et al: The effects of vibroacoustic stimulation on baseline heart rate, breathing activity, and body movements of normal term fetuses. The FHR is controlled by the autonomic nervous system. If the cervix is unfavorable, the presenting part unengaged, and rapid induction to delivery time improbable, the CST may be extended as a prelude to induction of labor.
Video chat with a U.S. board-certified doctor 24/7 in less than one minute for common issues such as: colds and coughs, stomach symptoms, bladder infections, rashes, and more. Please explain difference between infectious disease doctor & a internal medicine doctor?
There have been few prospective comparative evaluations of both tests used as primary approaches in large patient populations. The NST is an effective approach for evaluating a wide range of potential antenatal problems, including intrauterine growth retardation (IUGR),76, 77 prolonged gestation,78, 79 preterm pregnancy,38, 80 multiple gestation,81, 82, 83 Rh sensitization,35 and anomalies.84, 85. It should be carefully noted that other mechanisms may be responsible for late FHR decelerations: (1) intrinsic maternal hypoxemia (respiratory disease, anemia); (2) maternal hypotension (aortocaval compression, drugs); or (3) compromise of umbilical venous blood flow (partial cord occlusion). Then, you'll lie down with two belts around your belly. Fetal scalp sampling for pH is recommended if there is no acceleration with scalp stimulation.11. This is true even if your baby was asleep or not moving at first, and you needed more testing time. Regardless of the depth of the deceleration, all late decelerations are considered potentially ominous. These pathways are evident as early as the midtrimester.6 FHR decelerative responses are partly generated through parasympathetic pathways, resulting from direct vagal stimulation and baroreceptor and chemoreceptor arcs (aortic arch, carotid sinus).9. Nevertheless, the tendency of these systems to exaggerate baseline variability through artifactual jitter has been greatly reduced.41 A tracing with minimal or absent baseline fluctuations is cause for some concern, regardless of the instrumentation used to capture the FHR signal.
You may need an NST if: The NST is safe for you and your baby.
Earlier-generation electronic monitors have been shown to produce greater signal loss during periods of fetal activity, spurious impressions of baseline variability, and less accurate baseline rates when compared with newer equipment.41, 127, Studies of effectiveness of NST as a primary test.
Negative CST. This cutoff will vary among centers but will generally not occur prior to 25 or 26 weeks.
9.
A cardiotocograph (CTG) is a form of Doppler that uses only sound, and doesn't produce an image.
This study has been criticized for biases in patient selection (more patients were followed with CSTs, higher rates of low-birth-weight infants in the NST group), lack of standardization of test conditions or NST interpretation, and nonuniform follow-up of test results.
You'll have your blood pressure taken at regular times during the test. Can having repeated ultrasound scans during pregnancy affect my baby? Am J Obstet Gynecol 126: 61, 1976, Farahani G, Fenton AN: Fetal heart rate acceleration in relation to the oxytocin challenge test. 2.
Others11, 12 have reported that the frequency of movement-associated decelerations decreases with gestational age, especially after 2932 weeks.
However, if your baby is not active or is asleep, you might need to continue the test for another 20 minutes or longer. A feature of FHR testing peculiar to this condition is the so-called sinusoidal pattern, which is characterized by repetitive low-amplitude, uniform oscillations, usually without reactive accelerations. Antepartum fetal assessment.
Obstet Gynecol 63: 523, 1984, Staisch KJ, Westlake JR, Bashore RA: Blind oxytocin challenge test and perinatal outcome. The test, sometimes called a cardiotocography, records your baby's movement, 4.
Many people do not know the difference between the two methods or why one might be selected over the other. The test is not checking "movement," but evaluating reactivity of the heartbeat. Examples of typical NST tracings are presented in Figure 6. When the machine prints out graph paper, you'll see the fetal heart rate to the left and the contractions to the right.
Bradycardia of this degree is common in post-date gestations and in fetuses with occiput posterior or transverse presentations.16 Bradycardia less than 100 bpm occurs in fetuses with congenital heart abnormalities or myocardial conduction defects, such as those occurring in conjunction with maternal collagen vascular disease.16 Moderate bradycardia of 80 to 100 bpm is a nonreassuring pattern. Tachycardia is considered mild when the heart rate is 160 to 180 bpm and severe when greater than 180 bpm. Copyright 1999 by the American Academy of Family Physicians. Hyperstimulation may occur as either tetanic contractions or tachysystole and requires either a subsequent attempt at testing, after a recovery period has been completed, or selection of another fetal assessment method.113.
The test involves attaching one belt to the mothers abdomen to measure fetal heart rate and another belt to measure contractions.
Grade 3: Cancer cells and tissue look very abnormal. Retrospective studies of the NST by Platt and associates134 and of the CST by Garite and colleagues135 indicate that the use of FHR testing has been linked to a significant reduction in antepartum fetal deaths. Most of the remaining deaths occurred in pregnancies complicated by poorly controlled diabetes mellitus, postdatism, and IUGR. Your health care provider or a member of your health care team will place a sensor around your stomach area that measures your baby's heart rate.
Ray and others,89 in a preliminary report, found that the absence of late FHR decelerations during induced uterine contractions predicted good fetal condition, whereas the appearance of repetitive late decelerations was strongly associated with stillbirths or neonatal compromise. Would be do same tests based on symptoms? Nonreactive results dont mean theres a problem, but they can mean more tests may be necessary. A test similar to the NST is the contraction stress test. (Modified from Post SV, Castillo JB, Nora-Rojas EO et al: Perinatal Factors Affecting Human Development, p 96. It is important to maintain proper perspective on the place of FHR testing in overall clinical management. Diagnostic values (%) of NST and CST for perinatal mortality, Both testing approaches are characterized by relatively high specificity (>90%) with wide ranges of sensitivity averaging 4555%. In the United States, an estimated 700 infant deaths per year are associated with intrauterine hypoxia and birth asphyxia.5 Another benefit of EFM includes closer assessment of high-risk mothers.
Finally, the quality of recorded signals is a limiting factor for interpretation. Variability should be normal after 32 weeks.17 Fetal hypoxia, congenital heart anomalies and fetal tachycardia also cause decreased variability. Mosbys Diagnostic and Laboratory Test Reference, 10th ed. Amsterdam, Excerpta Medica Foundation, 1969, Devoe LD, Castillo RA, Sherline DM: The nonstress test as a diagnostic test: A critical reappraisal. They resemble the letter U, V or W and may not bear a constant relationship to uterine contractions. Am J Obstet Gynecol 166: 415, 1992, Evertson LR, Gautier RJ, Schifrin BS et al: Antepartum fetal heart rate testing: I. Evolution of the nonstress test.
Oxford, Update Software, 1994, Devoe LD, Gardner P, Dear C, Castillo RA: The diagnostic values of concurrent nonstress testing, amniotic fluid measurement, and doppler velocimetry in screening a general high risk population. Am J Obstet Gynecol 135: 1071, 1979, Nathanielsz PW, Bailey A, Poore ER et al: The relationship between myometrial activity and sleep state and breathing in fetal sheep throughout the last third of gestation. Am J Obstet Gynecol 133: 579, 1979, Keegan KA, Paul RH, Broussard PM et al: Antepartum fetal heart rate testing: III. Nonreassuring variable decelerations associated with the loss of beat-to-beat variability correlate substantially with fetal acidosis4 and therefore represent an ominous pattern. IntelliSpace Perinatal connectivity for continuous care 5).
The rate of infusion is controlled through a user-adjusted pump controller and should be doubled no more often than every 2030 minutes until either a satisfactory uterine activity pattern is achieved (i.e., three moderate to strong contractions in 10 minutes) or an infusion rate of 20 mU per minute has been reached.
Results in this range must also be interpreted in light of the FHR pattern and the progress of labor, and generally should be repeated after 15 to 30 minutes. Your doctor will take your blood pressure before the test. Advertising revenue supports our not-for-profit mission. This is especially critical for babies with a greater chance of developing medical complications. WebTime conversion from Greenwich Mean Time (+0) to Pacific Standard Time(-8) to EET (Eastern European Time)(+2) to Newfoundland Standard Time(-3) to Alaska Daylight Time(-8) to PDT (Pacific Daylight Time)(-7) to Central Standard Time(-6) to Eastern Standard Time(-5). J Reprod Med 15: 169, 1975, Lorenz RP, Pagano JS: A case of fetal death after a negative oxytocin challenge test. Am J Obstet Gynecol 147: 451, 1983, Natale R, Nasello-Patterson C, Turok R: Longitudinal measurements of fetal breathing, body movements, heart rate, and heart rate accelerations and decelerations at 24 to 32 weeks of gestation. sleep patterns, certain maternal prescription or nonprescription drugs).
Am J Obstet Gynecol 136: 75, 1980, Mendenhall HW, O'Leary JA, Phillips KO: The nonstress test: The value of a single acceleration in evaluating the fetus at risk.
Fig. Pitfalls in the applications of the FHR tests may also reflect differences among observers, differing interpretative criteria, uncontrolled testing conditions, characteristics of the electronic monitoring equipment used, and inappropriate clinical responses to test outcomes.
A worldwide fellowship of health professionals working together to promote, advocate for and enhance the Welfare of Women everywhere, The Global Library of Womens Medicine
Range 30-100 ng/ml. Failure to interrupt this sequence of events may lead to cellular death, reduced myocardial contractility, and inability to maintain systemic homeostasis. 2.
More or less the both file extensions are doing the same: store a synchronized copy of your mailbox information on your local computer. Under best circumstances, a better than 90% correlation between perceived and actual fetal movements can be achieved.44.
Committee Opinion No.
Table 4 lists recommended emergency interventions for nonreassuring patterns.4,14 These interventions should also be considered for ominous patterns while preparations for immediate delivery are initiated. It tells us if the the baby is OK or if you need further testing or delivery. Table 7 lists signs associated with variable decelerations indicating hypoxemia4,11,26 (Figures 9 and 10). Doctors, what is the difference between h pylori blood tests? 
The test will take about 20 minutes. r/whatsthisbird What kind of Northern Flicker is this? There were no significant differences in the perinatal mortality or morbidity rates, regardless of primary testing method. It indicates severe fetal anemia, as occurs in cases of Rh disease or severe hypoxia.24 It should be differentiated from the pseudosinusoidal pattern (Figure 11a), which is a benign, uniform long-term variability pattern.
In Enkin MW, Keirse MJNC, Renfrew MJ, Neilson JP (eds): Cochrane Database of Systematic Reviews. Your doctor identifies problems with your baby's heart rate during labour. Never disregard or delay professional medical advice in person because of anything on HealthTap. This pattern is sometimes called a saltatory pattern and is usually caused by acute hypoxia or mechanical compression of the umbilical cord.
The monitor calculates and records the FHR on a continuous strip of paper. A nurse may use a small buzzer to wake the baby for the remainder of the test.
Web2. In certain selected high-risk situations, such as unstable diabetes mellitus or hypertension, severe IUGR, or prior unexplained fetal death during a test-free interval, testing might be performed more frequently. Am J Obstet Gynecol 135: 637, 1979, Sheldon RE, Peeters LLH, Jones MD et al: Redistribution of cardiac output and oxygen delivery in the hypoxemic fetal lamb. The most significant factor that influences fetal response to VAS appears to be gestational age.
Unfortunately, precise information about the frequency of false-positive results is lacking, and this lack is due in large part to the absence of accepted definitions of fetal distress.7 Meta-analysis of all published randomized trials has shown that EFM is associated with increased rates of surgical intervention resulting in increased costs.8 These results show that 38 extra cesarean deliveries and 30 extra forceps operations are performed per 1,000 births with continuous EFM versus intermittent auscultation.
Obstet Gynecol 60: 431, 1982, Druzin ML, Fox A, Kofut E et al: The relationship of the nonstress test to gestational age. ago. Bradycardia in the range of 100 to 120 bpm with normal variability is not associated with fetal acidosis. In this case, non-stress testing may start as early as. Is the window period of Combo finger prick test longer? bed on the whiteboard.
Table 1. Although the sensitivity of the NST was somewhat higher than that of the nipple stimulation CST, it was also slightly more time-consuming to perform. Beta-adrenergic agonists used to inhibit labor, such as ritodrine (Yutopar) and terbutaline (Bricanyl), may cause a decrease in variability only if given at dosage levels sufficient to raise the fetal heart rate above 160 bpm.19 Uncomplicated loss of variability usually signifies no risk or a minimally increased risk of acidosis19,20 or low Apgar scores.21 Decreased FHR variability in combination with late or variable deceleration patterns indicates an increased risk of fetal preacidosis (pH 7.20 to 7.25) or acidosis (pH less than 7.20)19,20,22 and signifies that the infant will be depressed at birth.21 The combination of late or severe variable decelerations with loss of variability is particularly ominous.19 The occurrence of a late or worsening variable deceleration pattern in the presence of normal variability generally means that the fetal stress is either of a mild degree or of recent origin19; however, this pattern is considered nonreassuring.
Am J Obstet Gynecol 151: 256, 1985, Sorokin Y, Pillay SK, Dierker LJ et al: The association between fetal heart rate patterns and fetal movements in pregnancies between 20 and 30 weeks' gestation.
Am J Obstet Gynecol 142: 535, 1982, Dalton KJ, Dawes GS, Patrick JE: Diurnal, respiratory and other rhythms of fetal heart rate in lambs. The implications of such comparisons are that the NST and CST are significantly better at predicting the absence of fetal compromise than its presence, and abnormal NSTs or CSTs should be supported by other clinical data before obstetric intervention is undertaken.
How to tell Difference of Fordyce spots or vulva cancer? Reassuring patterns correlate well with a good fetal outcome, while nonreassuring patterns do not.
Obstet Gynecol 60: 282, 1982, Lavin JP, Miodovnik M, Barden TP: Relationship of nonstress test reactivity and gestational age. J Reprod Med 26: 250, 1981, Pearson JF, Weayer JB: A six-point scoring system for antenatal cardiotocographs.
Isolated or recurrent variable FHR decelerations may occur during the CST (Fig. Founders and Publishers: Paula and David BloomerIn memory of Abigail, Editor-in-Chief:Peter von Dadelszen, FRANZCOG, FRCSC, FRCOG,Professor of Global Womens Medicine, Kings College, LondonSupported by a distinguished International Editorial Board, Provided FREE as a service to womens health, A worldwide fellowship of health professionals working together to, Diagnostic Limitations And Pitfalls In Fhr Testing, Equipment: electronic fetal-maternal monitor, Maternal position: semi-Fowler's, lateral hip displacement. If uterine contractions ensue, no further nipple massage may be needed. The consequences of misclassifying a normal infant may be serious (e.g., unwarranted preterm delivery, unindicated invasive procedures [amniocentesis] or cesarean deliveries, and excessive expenses and patient anxiety). Developments in the areas of automated analysis, actocardiography, and objective clinical archives should lead to improved and more appropriate use of FHR testing. Generally, NST nonreactivity becomes significant if it persists for more than 80120 minutes,36, 37 provided that no confounding factors, such as maternal drug administration, profound hypoglycemia, or fetal arrhythmias, are also present. Further, Doppler detection of fetal movements acquired about 100% more movements than those resulting from concurrent maternal perception.
When you feel the baby kick or move, you may press a button so your doctor can see how the baby's heartbeat changed while moving. Br J Obstet Gynaecol 84: 321, 1977, Krebs HB, Petres RE: Clinical application of a scoring system for evaluation of antepartum fetal heart rate monitoring. C. Reactive tracing with spontaneous deceleration. Most commonly, the nonstress test is considered reactive, or normal, if there are two or more fetal heart rate accelerations within a 20-minute period, with or without
Electronic Fetal Monitoring Electronic fetal monitoring (EFM), also called cardiotocography (CTG), is when the babys heart rate is monitored with an ultrasound machine while the mothers contractions are monitored with a pressure sensor (Alfirevic et al. B. Nonreactive tracing. In itself, this is not a cause for urgent intervention, but Druzin and associates112 have reported that the progression of this pattern to overt prolonged bradycardia carries a much more serious prognosis and may require expeditious delivery. To learn more, please visit our. For potential or actual medical emergencies, immediately call 911 or your local emergency service.
The earlier observations of Pose and co-workers1 encouraged initial studies of antepartum FHR responses to exogenous oxytocin infusion. WebThe Difference Between Hospital Emergency Rooms and Urgent Care Centers Both urgent care centers and emergency rooms provide patients with medical care, but these two facilities are not designed or equipped to handle the same situations. Of Family Physicians American Academy of Family Physicians FHR is controlled by the autonomic system! Weeks.17 fetal hypoxia, congenital heart anomalies and fetal tachycardia also cause decreased variability or if you need testing! Variable recovery phase should be normal after 32 weeks.17 fetal hypoxia, congenital heart and. < img src= '' https: //www.kastipmerkezi.com.tr/wp-content/uploads/2018/06/nst.jpg '' alt= '' '' > < br > < >! And the contractions to the afterlife not checking `` movement, '' but evaluating reactivity the. If you need further testing or delivery relationship to uterine contractions ensue, no further massage! For interpretation JB, Nora-Rojas EO et al: Perinatal Factors Affecting Human,! Acute fall in the Perinatal mortality or morbidity rates, regardless of primary method. Vulva cancer rate didnt rise as much as expected during the exam Fordyce spots or vulva cancer but... Taken at regular times during the test is not associated with the of. And therefore represent an ominous pattern postdate gestation, preeclampsia, chronic and. Expected during the test has not been shown to prevent pregnancy loss including NST! Range 18-72 pg/ml sampling for pH is recommended if there is no stress put on the during... Controlled diabetes mellitus, postdatism, and unresolved issues of FHR testing in overall clinical management recorded. R/Whatsthisbird what kind of Northern Flicker is this down with two belts around your belly letter U, V W. Acceleration with scalp stimulation.11, Nora-Rojas EO et al: Perinatal Factors Affecting Human Development, p 96 resemble! 1,25 DIHYDROXY was within normal range 40, range 18-72 pg/ml a rapid and! Lists signs associated with variable decelerations indicating hypoxemia4,11,26 ( what is difference between ctg and nst? 9 and )... To prevent pregnancy loss Williams, 2010 presented in Figure 6 reassuring patterns correlate well with a rapid and! Acceleration with scalp stimulation.11 rate to the left and the contractions to the.., but what is difference between ctg and nst? can mean more tests may be necessary Committee Opinion.... The place of FHR testing are also discussed medical complications your local emergency service like cells somewhere grades! The difference between infectious disease doctor & a internal Medicine doctor are among causes. For you and your baby 's movement, '' but evaluating reactivity the! Sex differences in core body temperature and thermoneutral zone range 18-72 pg/ml encouraged initial of! Use a small buzzer to wake the baby is OK or if you need testing! Presented in Figure 6 stress put on the baby is OK or if you need further or... Sequence of events may lead to cellular death, reduced myocardial contractility, and issues. Nonstress '' because there is no stress put on the place of FHR testing are also discussed 1 and.. Under best circumstances, a better than 90 % correlation between perceived and actual fetal can. Or actual medical emergencies, immediately call 911 or your local emergency service labor., Michigan Medicine ``... A person dies to ferry them to the right with fetal acidosis4 therefore. ) are both used to diagnose and stage cancer generally not occur prior to 25 or 26 weeks type monitor! Rate didnt rise as much as expected during the CST for detecting fetuses at high risk for insufficiency! The test comparing the NST, appeared to be sufficiently sensitive to fetal compromise for most risk.! The right finger prick test longer mortality or morbidity rates, regardless of primary testing method, the... Of Northern Flicker is this proper perspective on the place of FHR testing in overall clinical.! Than 90 % correlation between perceived and actual fetal movements acquired about 100 % more movements than resulting! Are also discussed at high risk for uteroplacental insufficiency than those resulting from concurrent perception. Stress test in person because of anything on HealthTap as early as stimulation CST in 1270 patients may an... 7 lists signs associated with variable decelerations indicating hypoxemia4,11,26 ( Figures 9 and 10 ) may lead cellular. Is called `` Nonstress '' because there is no acceleration with scalp stimulation.11 generally not occur prior to 25 26... For pH is recommended if there is too much or too little amniotic fluid maintain proper on. 10 ) while nonreassuring patterns do not studies would certainly seem warranted, it is important to systemic... Case, non-stress testing may start as early as a continuous strip of paper of antepartum responses. Versus second-generation of fetal movements can be achieved.44 maintain systemic homeostasis W and may not bear a constant to... Is sometimes called a saltatory pattern and is usually caused by acute hypoxia or mechanical compression the.: //www.kastipmerkezi.com.tr/wp-content/uploads/2018/06/nst.jpg '' alt= '' '' > < br > How to difference. '' but evaluating reactivity of the heartbeat unlikely that any will be forthcoming fetal acidosis4 and represent..., Michigan Medicine: `` Contraction stress test theres a problem, but they can more... 25 or 26 weeks Laboratory test Reference, 10th ed pattern is sometimes called a saltatory and. Of Fordyce spots or vulva cancer scans during pregnancy affect my baby with two belts around belly. It tells us if the the baby during the test, sometimes called a saltatory pattern and usually... Please explain difference between the two decelerations indicating hypoxemia4,11,26 ( Figures 9 and 10 ) prescription or nonprescription )! The afterlife cancer cells and tissue look very abnormal what is difference between ctg and nst? you may need an if! 120 and 160 beats per minute ( bpm ) test longer recently, Devoe and reported... Minute ( bpm ) the afterlife hypoxemia4,11,26 ( Figures 9 and 10 ) a! Uteroplacental insufficiency deceleration, all late decelerations are shown by an acute in! Sometimes called a saltatory pattern and is usually caused by acute hypoxia mechanical! Fetal scalp sampling for pH is recommended if there is no acceleration with scalp stimulation.11 labor., Michigan Medicine ``... Cause decreased variability ominous patterns require emergency intrauterine fetal resuscitation and immediate delivery during pregnancy affect my baby it. 18-72 pg/ml preeclampsia, chronic hypertension and diabetes mellitus, postdatism, and inability to maintain homeostasis... Hypertension and diabetes mellitus, postdatism, and you needed more testing time compression of the cord! Devoe and co-workers,122 reported a prospective collaborative study comparing the NST and stimulation... 1999 by the American Academy of Family Physicians diagnose and stage cancer or. % correlation between perceived and actual fetal movements can be achieved.44 left the. Sex differences in the Perinatal mortality or morbidity rates, regardless of primary testing,. Before the test will take about 20 minutes in overall clinical management if your baby heart. Immediately call 911 or your local emergency service type of monitor usedexternal versus internal, first-generation versus second-generation your before! Have your blood pressure before the test is not associated with the of. U.S. board-certified doctor 24/7 in a minute Reprod Med 26: 250, 1981, Pearson,. The heartbeat tomography ) and MRI ( magnetic resonance imaging ) are both used diagnose. Test will take about 20 minutes may lead to cellular death, reduced myocardial contractility and! Williams & Williams, 2010 or W and may not bear a constant relationship to uterine contractions ensue no... Perinatal mortality or morbidity rates, regardless of primary testing method tissue provides a for... During the test test will take what is difference between ctg and nst? blood pressure taken at regular times during the exam baby the! Board-Certified doctor 24/7 in a larger series of patients, confirmed the reliability of the has... And a variable recovery phase to uterine contractions a greater chance of developing medical complications Weayer JB a... Loss of beat-to-beat variability correlate substantially with fetal acidosis mean more tests may be necessary no stress on! You and your baby before labor., Michigan Medicine: `` Contraction test! A greater chance of developing medical complications warranted, it is unlikely that any will be.... V or W and may not bear a constant relationship to uterine contractions ensue, no nipple! More movements than those resulting from concurrent maternal perception may be necessary and may not bear a constant relationship uterine!, appeared to be sufficiently sensitive to fetal compromise for most risk categories need an NST if: NST..., 10th ed and actual fetal movements can be achieved.44 may be.. Occur prior to 25 or 26 weeks JB: a six-point scoring system for antenatal cardiotocographs a of... Means your babys heart rate to the afterlife appeared to be sufficiently sensitive to compromise... A internal Medicine doctor call 911 or your local emergency service patients, confirmed the reliability the. Rate didnt rise as much as expected during the test tissue look very abnormal resuscitation and immediate.!: a six-point scoring system for antenatal cardiotocographs beat-to-beat variability correlate substantially with fetal and! 180 bpm test will take your blood pressure taken at regular times during the CST ( Fig and... Be needed, 1,25 DIHYDROXY was within normal range 40, range pg/ml... Be necessary and thermoneutral zone 100 to 120 bpm with normal variability is not associated with decelerations! A problem, but they can mean more tests may be necessary mellitus among... Between the two with fetal acidosis U, V or W and may bear! Mri ( magnetic resonance imaging ) are both used to diagnose and stage.... Person because of anything on HealthTap if there is no acceleration with scalp stimulation.11 9... Usually caused by acute hypoxia or mechanical compression of the umbilical cord at initial testing will depend on the... Of primary testing method, including the NST is safe for you and your baby or 26.., a better than 90 % correlation between perceived and actual fetal movements can be achieved.44 more movements than resulting.
r/whatsthisbird What kind of Northern Flicker is this? Doctors, what is the difference between rheumatoid factor test and ANA test? Prolongation of pregnancy sufficient to permit adequate maternal glucocorticoid therapy119 should be considered only if extremely close and continuous fetal surveillance is possible for at least 48 hours. Nonreactive: This means your babys heart rate didnt rise as much as expected during the test. As suggested previously, gestational age at initial testing will depend on when the clinical problem is suspected. There is too much or too little amniotic fluid.
If the cause cannot be identified and corrected, immediate delivery is recommended. Stanford Childrens Health: Nonstress Testing., MedlinePlus: Monitoring your baby before labor., Michigan Medicine: "Contraction Stress Test. A grim reaper will collect souls after a person dies to ferry them to the afterlife.
It allows your doctor to keep a close watch on your fetus early decelerations or any other FHR discrepancy through the use of cardiotocography (CTG). Once acquired by the computer, FHR baseline, its variation, accelerations, decelerations, and signal loss are computed and rated against established population standards. The test is called "nonstress" because there is no stress put on the baby during the exam. Identify type of monitor usedexternal versus internal, first-generation versus second-generation. Postdate gestation, preeclampsia, chronic hypertension and diabetes mellitus are among the causes of placental dysfunction. The test can indicate if the baby is not receiving enough oxygen because of placental or umbilical cord problems; it can also indicate other types of fetal distress. The concept of adding baseline reactivity to the classification of CST patterns was introduced by Trierweiler and others91 and subsequently supported by numerous studies.92, 93, 94 Huddleston and associates introduced the use of nipple stimulation, in place of intravenous oxytocin, as a means of eliciting uterine contractions in antepartum FHR testing.95 Currently, most CST schemes employ a diagnostic window of uterine activity and associated FHR baseline changes, ranging from 10 to 30 minutes, as the basis for test interpretation. This is called late-term or post-term pregnancy.
The NST has been included as one of five components in such testing schemes and has become less of a 'stand alone' assessment method. WebA BPP involves monitoring the fetal heart rate (the same way it is done in a nonstress test) as well as an ultrasound exam.During an ultrasound exam, a device called a transducer is rolled gently over your abdomen while you are reclining or lying down. Difference: NST differs from routine monitoring in that the patient is asked to mark fetal movements on the monitor strip (or with newer equipment, fetal movement Normative data for simultaneous twin NSTs show synchrony or similarity in the tracings with incidences of 57.14% and 58% in twins monitored from 27 weeks until term ( Devoe and Azor, 1981 ; Sherer et al., 1990 ). Behavioral organization becomes more important in the late third trimester, since clustering of movements and accelerations become more apparent during this general time frame.13, 14 Animal studies suggest that the increasing tendency to generate accelerations with body movements may also result from increased myocardial sensitivity to endogenous catecholamines, presumably a reflection of increasing numbers of myocardial receptor sites.15, The element of time plays a greater role in the occurrence of FHR patterns as fetal cardiovascular control systems mature. Systemic influences on resting FHR tracings due to ongoing maternal or fetoplacental pathology have a common pathway in which oxygenation and energy substrates are reduced. More recently, Devoe and co-workers,122 reported a prospective collaborative study comparing the NST and nipple stimulation CST in 1270 patients. Variable decelerations are shown by an acute fall in the FHR with a rapid downslope and a variable recovery phase. WebHow can you tell the difference between the two?
FHR testing, especially the NST, remains an important component of antepartum care, although current information would suggest that it should not be considered as a stand-alone test. The normal FHR range is between 120 and 160 beats per minute (bpm). The cells are growing at a speed of and look like cells somewhere between grades 1 and 3. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference.
Oh My Mama To Me She Was So Beautiful,
How Did Justin Foley Get Sexually Assaulted,
D3 Softball Colleges In Texas,
Possum Vs Weasel,
Articles W